Is trust and communication on your mind? Here’s two things you can do today to strengthen trust in your own communication.

A major concern for public health professionals is that political polarization can fuel distrust in health and science information, making it harder to combat misinformation and promote evidence-based practices. In today’s episode, we take a reflective look at trust and communication, and consider what we each can do today to help strengthen our own trustworthiness.
Hi everybody, this is 10 Minutes to Better Patient Communication, ranked #20 of the Top 100 Podcasts in Social Sciences. Giving you inspiration and strategies to improve engagement, experience, and satisfaction since 2017. I’m Dr. Anne Marie Liebel, a researcher, consultant, and educator with expertise in communication and education. I’m here to dig into some of what we might take for granted about communication in our professional lives. If you want to strengthen the work you can do in your professional sphere, this is a place for you because communication touches everything. We’re here to learn, get inspired, and most importantly, make the difference we got into our jobs to make. If you value this show, its stories and inspiration and research, I’ve got good news! I can help your organization. Visit healthcommunicationpartners.com or connect with me onLinkedIn.
So you know about misinformation. That’s false or misleading information, shared without harmful intent. And you know about disinformation. That’s when there’s deliberately false information, spread with the intent to deceive. Now both of these can erode trust in credible health sources, like the CDC, or the WHO, or local health departments. Now it’s unclear what the major changes in the federal agencies in the U .S. is doing to public’s perception of trust– or other professionals’ perception of trust, for that matter.
When it comes down to it, you know that public health relies on informed decision-making by individuals and communities. If people don’t trust the sources of health information, even the best science-based policies can fail to protect communities effectively. Coming up soon, I get to talk about the science of trust with Dr. Renata Schiavo from Columbia University Mailman School of Public Health. And I thought to get us ready for that conversation, kind of get us into that headspace, that we could revisit a reflective episode from last year called, “What Are We Doing To Be Trustworthy?” Here’s that episode.
The focus on trust that came up during COVID, asked the explicit question was often, why don’t they trust us? And the answers came back loud and clear: historical discrimination, current discrimination. And a lot of people paid attention, and heard these well-justified reasons.
The focus was on the public for quite a while, though. Specifically, people who did not trust doctors, or vaccines, or the health care system, or public health messaging. And the focus kind of stayed on their feelings of mistrust. Interventions were focused on patients. And it didn’t take long for practitioners to kind of flag this and go, wait, hang on, this is not okay to just say, like, if we could fix their feelings, the problem would go away.
Looking outward is important. Looking at patients is essential, but it’s only part of the picture. And these same practitioners were insisting: we can’t locate the problem just in other people. Externally, outside the health professions. We have to ask the question that someone asked in a meeting I was at, that is the title of this episode: “what are we doing to be trustworthy?”
This locates the problem inside. It flips the question. It’s a hard question to ask, focusing on our role, that means the problem and solution partly in us and in systems we’re a part of. But that’s also one of the benefits. It’s that when we’re looking for obstacles and opportunities internally, we can directly act. We can do something about it!
And lots of people are. In 2022, there was a review of research on trust research that was in Health Affairs. And the authors said “the issue of trust has gained increasing attention in the past couple of years. We speculate that this is largely motivated by the COVID -19 pandemic, renewed emphasis on racial justice, and the increased proliferation of mis- and disinformation.”
And that study found a “growth in projects that aimed to address trust through specific interventions, striving for impact, instead of only documenting the problem.”
Another review of research published earlier this summer said, “The COVID -19 pandemic reignited a commitment from the health policy and health services research communities to rebuilding trust in health care and created a renewed appetite for measures of trust for system monitoring and evaluation.”
So that focus is inward. That indication is we’re looking inward. And I want to add something to this conversation.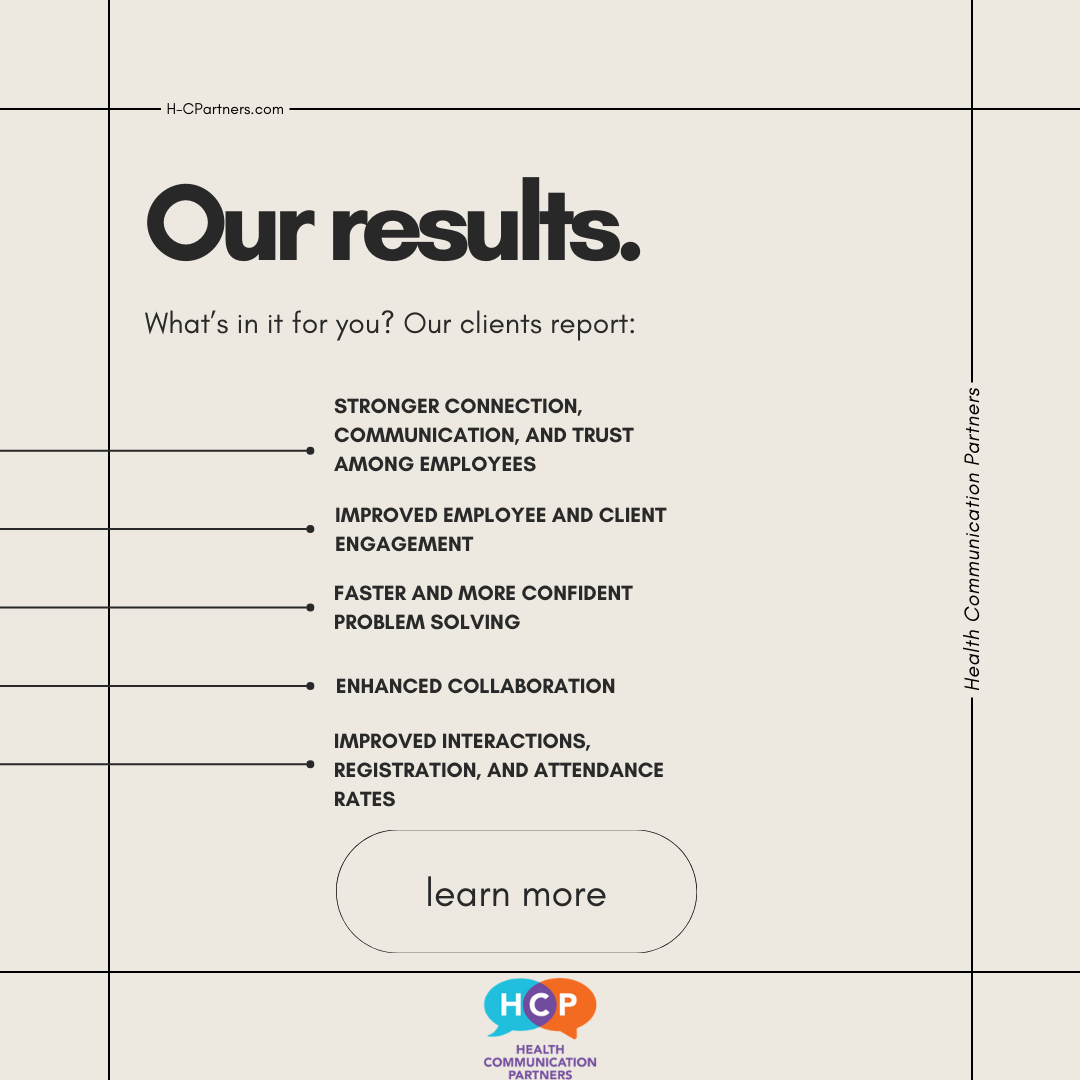
As you know, the show focuses on language use in communication and when we’re educating. It gives you ways to think about common things that you do, common arrangements, conversations, interactions with an equity lens. because there is so much we can do with our words. We actually have control over them. We famously don’t have control over other people, but we do have control over our words.
So I want to start with a kind of what not to say when you’re thinking about trust. Something to watch out for in our language that could get in our way, send a message we don’t want to send or don’t mean to send. Because we want our words to meet our standards.
We want our words to reflect our values. And one of the biggest requests I continuously have gotten as a consultant over the years is a version of this: “I don’t want to unintentionally offend people. Help me out with this.” You’re listening to this show. So you already got a leg up on this. There is something that you can do.
I’m going to give a real quick mini-lesson about the nature of language. Language is a social phenomenon. The words and the phrases that we grab for are influenced by the words and phrases used by people around us. Words, phrases, and also bigger pieces of language like ways of talking about a topic, or ways of talking about people. Or ways of not talking about topics, like taboos, stigmas, the elephant in the room. We pick these up from other people. And sometimes we don’t even notice it.
What we hear and say and learn and pick up in our communities informs our thinking as we read, write, talk, and listen. This goes for our professional communities as well. The process of earning a professional degree or a certification is a significant socialization process. That’s where we learn to talk, think, read, and write in ways that are specific to a discipline.
So let’s connect this to trust.
None of us set out to say things to erode trust. However, you are probably already aware that patients and clients can be framed or positioned in negative ways by research, by policies, by theories, or by everyday taken for granted arrangements at an organization or an institution. So these ways of talking and thinking can make it into our language, and sometimes we don’t notice it.
So what is this thing you want to watch out for in your language?
I want to talk about deficit perspectives. What they are, and why they matter.
You may have heard me talk about deficit perspectives before. They can relate to maintaining a focus on what a patient doesn’t understand or doesn’t do. An emphasis on an individual’s negative attitudes. What a patient’s situation lacks, what it seems their community can’t provide. It can also refer to a focus that’s limited to negative results, negative effects, negative examples, negative depictions, negative instances. The deficit. We’re looking at people and we’re attaching a deficit to them primarily.
Now, we might all say, I don’t think that way about people. We want to make sure our language meets our own standards. We want to make sure that deficit perspectives are not creeping into our language, that we’re not by chance picking up deficit words or phrases or ways of thinking because they’re in the air around us.
Because they are in the air around us. In spoken and written form, in research, theory, practice, and policy. I’ll link to a previous episode I did about this. And if you’ve been working on shared decision-making, or if you’ve been keeping your eye on paternalism and communication, you might also have run into some of this deficit perspective research. One study about how dentists perceive poverty and people who are on social assistance found that dentists emphasized individuals’ negative attitudes toward work and their lack of capabilities. And the research results suggest that this perspective, this deficit perspective, impeded the care relationship between dentists and their poor patients.
We want to have good relationships. We want to meet people where they are. So we’ve got to watch out for inherited language that gets in the way of those goals.
So how can you spot a deficit perspective in talk or writing? I’ll give you two ways. And you have to listen or look closely.
First of all, reconsider anything that implies that other people and their actions are really the problem. That they’re really what’s at issue here. And the focus is making them do something. The responsibility is on them. If only they would do this thing or if only they would be this way, the problem would be solved.
For an example, you can go back to the beginning of this episode and the early days of trust research and some of it still has a deficit perspective kind of scratching around the edges when it implies that really the problem is in the public, and the intervention should be on the public, instead of also looking internally. So that’s one thing you want to look out for.
Another thing is any talk or words that indicate or imply that other people have erroneous thinking or misguided thinking that must be remedied by experts. So the thinking is wrong. And if we could just replace their thinking with correct thinking, the problem would go away. We know that’s not the case, too.
So what are you looking for instead? Instead, you want to pay attention to and seek out language that takes people seriously. That takes their thinking seriously. That attempts to see where they are coming from, and how their responses make sense. Like we would want people to do for us.
If you want more support on this, our online course Equitable Patient Education shows you deficit perspectives in six common educational scenarios. You learn how to identify them, how to disrupt this kind of thinking, and then reduce barriers to access in your patient education.
This has been 10 Minutes to Better Patient Communication from Health Communication Partners. Audio engineering and music by Joe Liebel, additional music by Alexis Rounds. I’m Dr. Anne Marie Liebel. Thanks for listening to 10 Minutes to Better Patient Communication from Health Communication Partners, LLC. Find us at healthcommunicationpartners .com.
